Template For Hospital Discharge
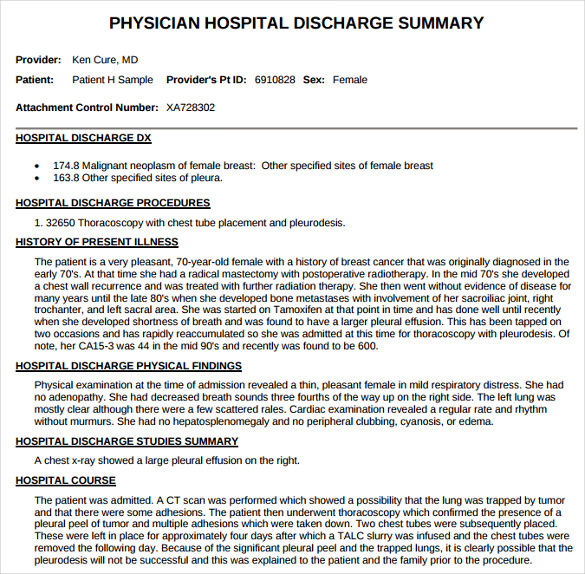
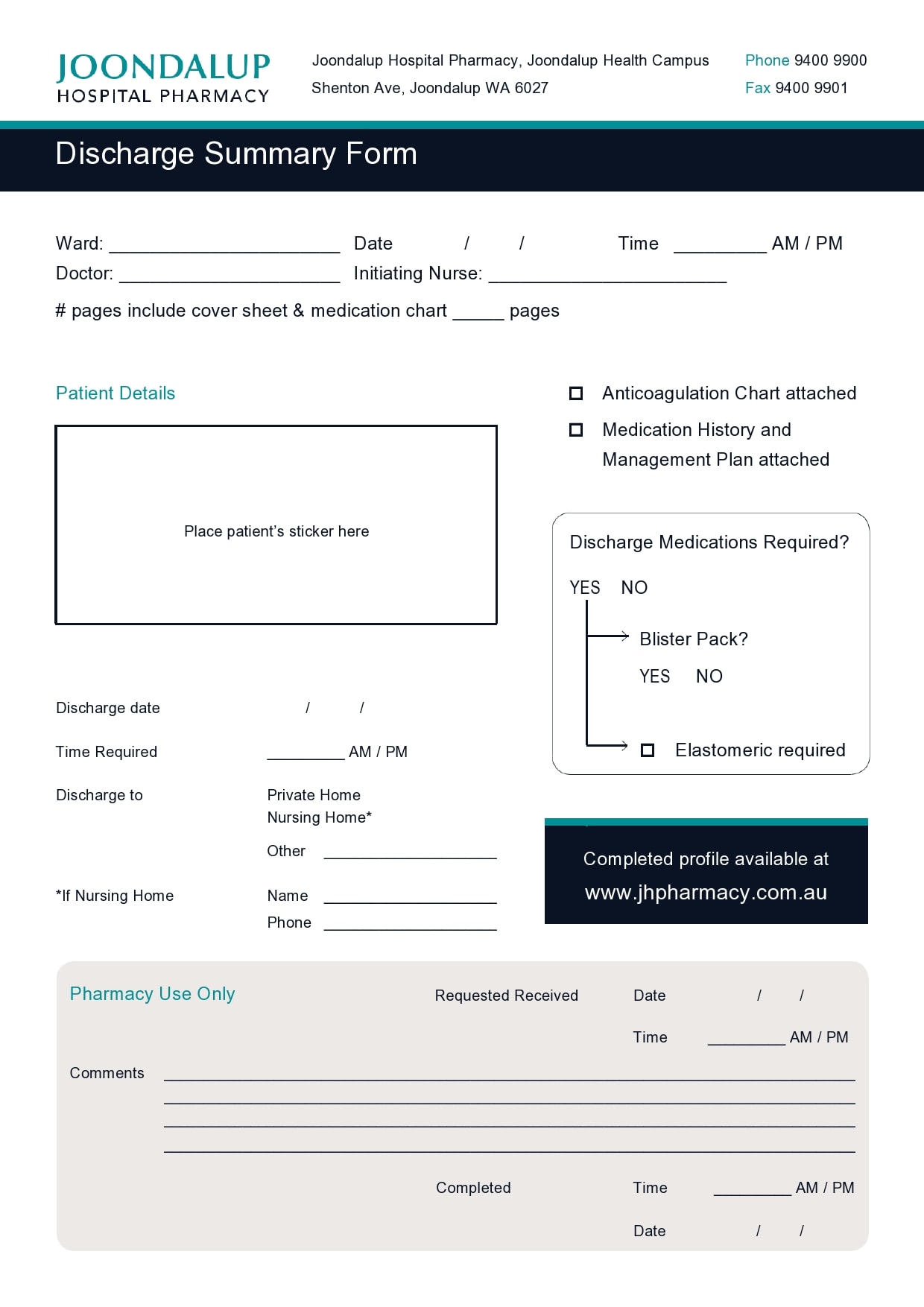
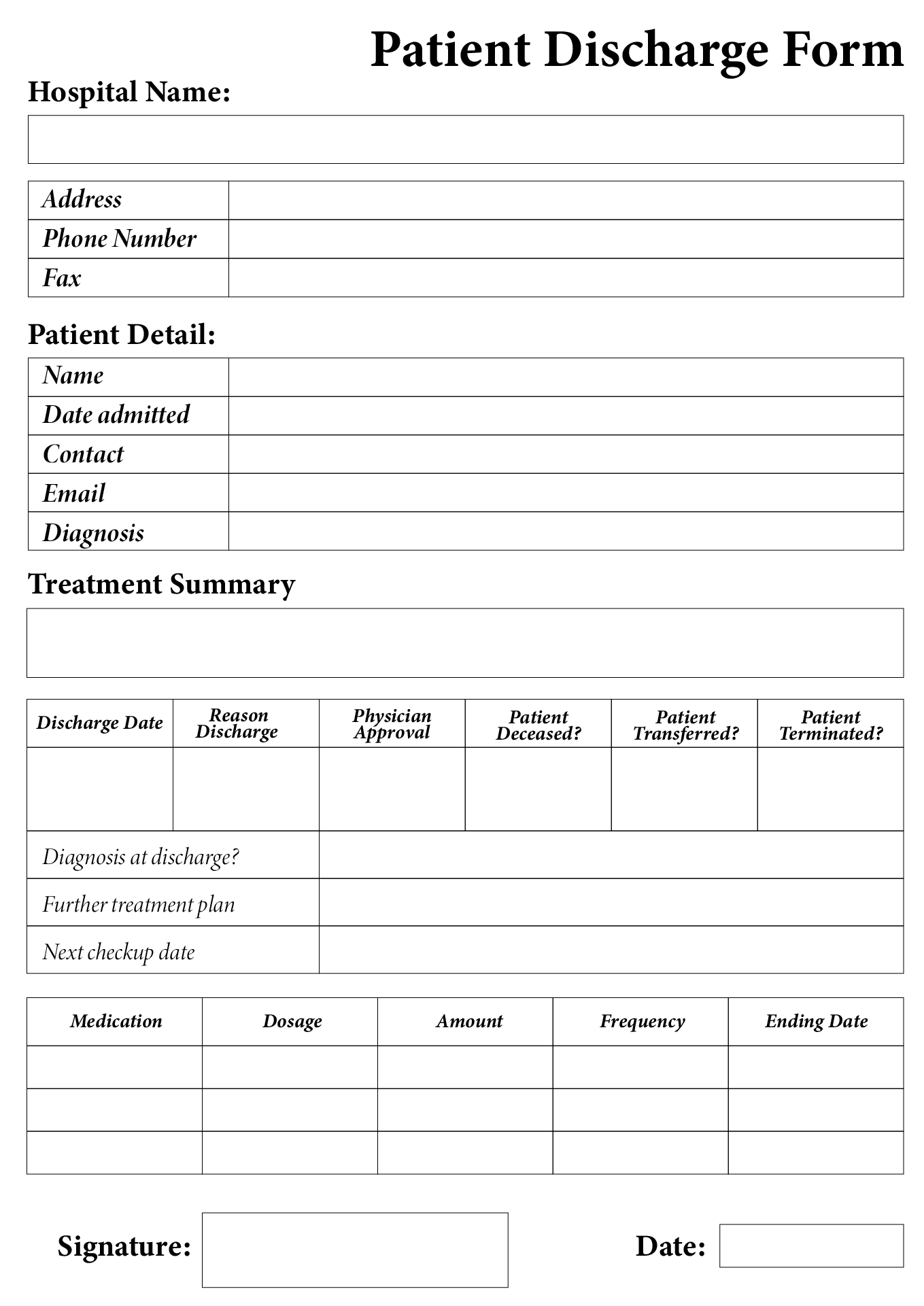
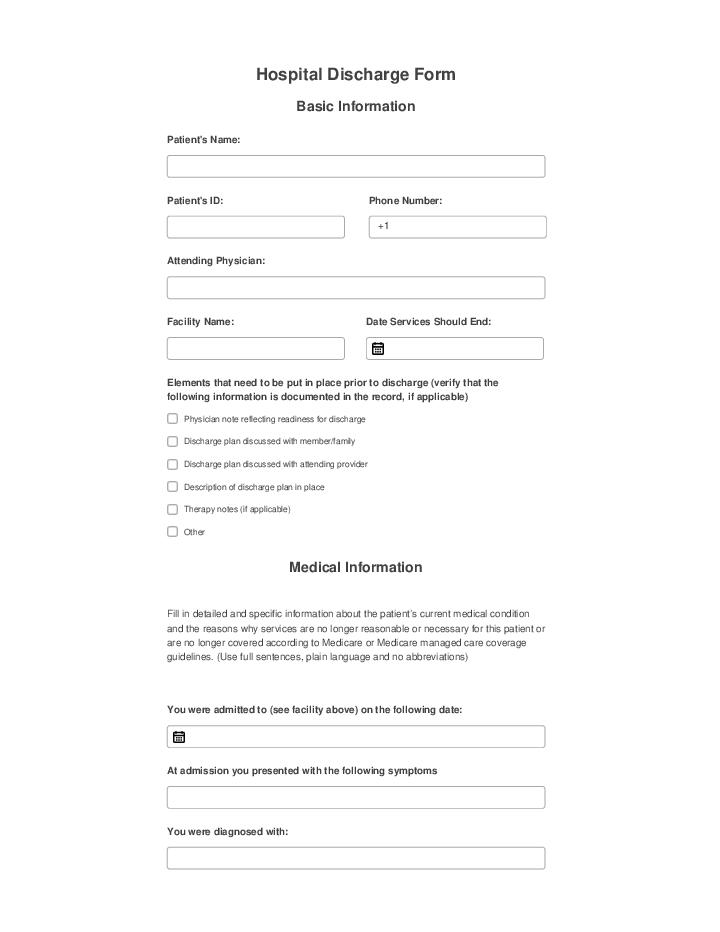
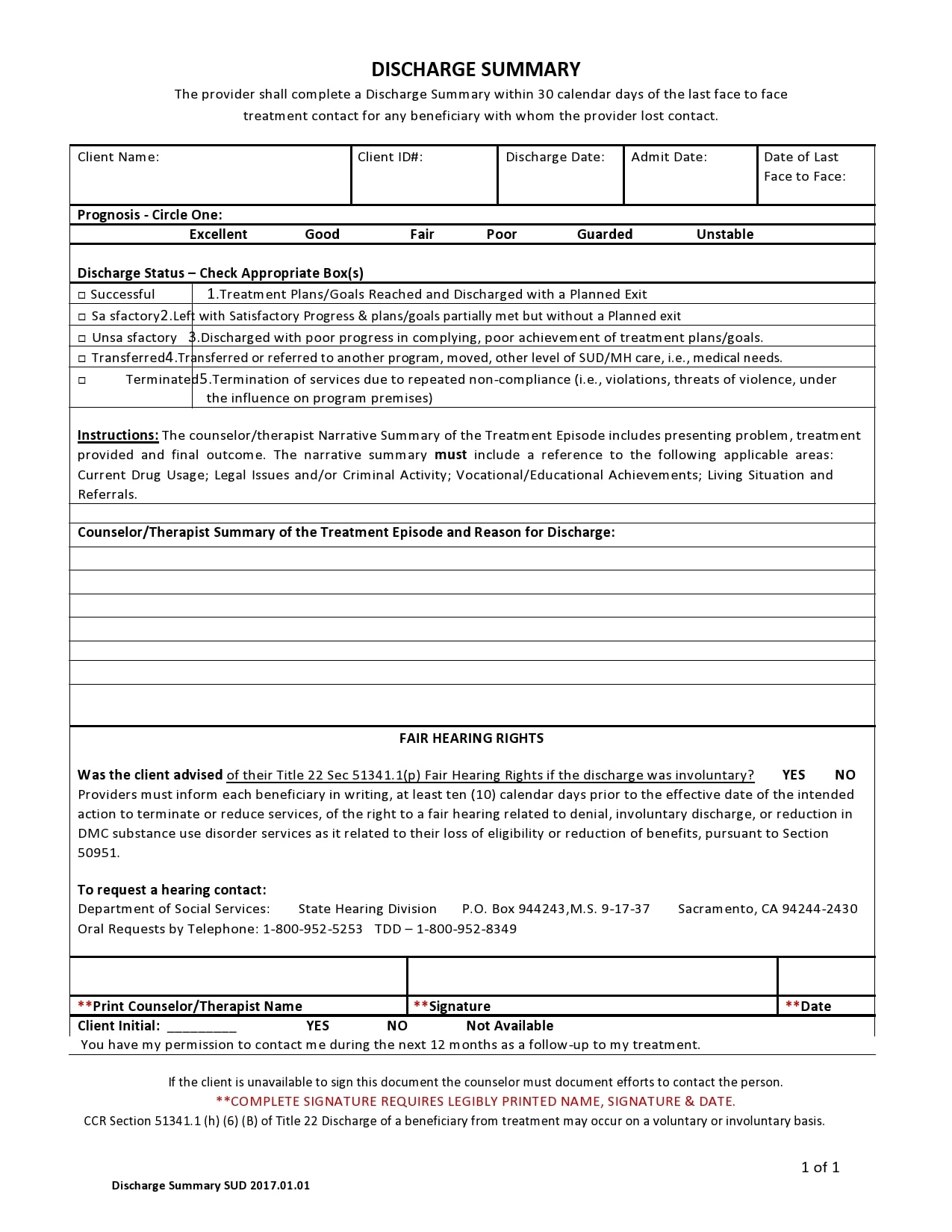
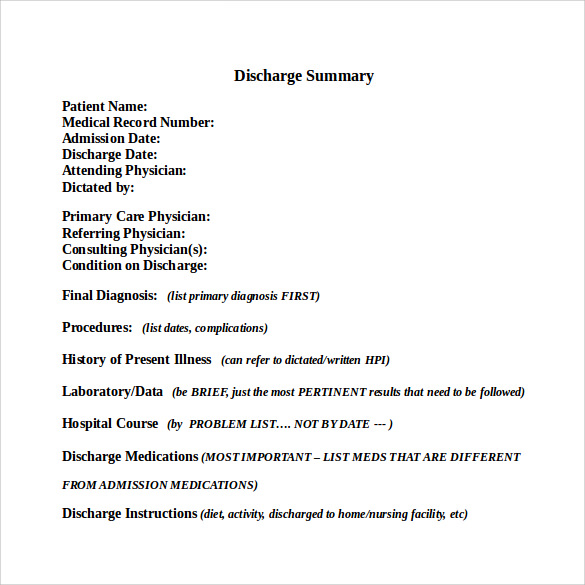
Template For Hospital Discharge - Discharge summary dictated 2 days after discharge states patient went “home”. A patient discharge form, sometimes referred to as a patient discharge summary, is a document issued by a hospital to an admitted patient upon discharge. If the patient was admitted or transferred to. This document not only outlines. A hospital discharge papers template typically includes several key components, such as patient demographics, admission and discharge. A summary discharge is a comprehensive clinical report prepared by a healthcare professional, typically a physician, nurse, or social worker, at the conclusion of a patient's. Hospital discharge papers template overview. A hospital discharge form is a form template designed to document patient discharge information and provide evidence of the patient's release from. Physician note on day of discharge further clarifies that the patient will be going home with. When a loved one is discharged from the hospital, receiving a comprehensive discharge summary is essential for a smooth transition home. Let’s review how to create effective discharge summaries and. Discharge summary forms are usually completed during a patient’s hospital stay and contain essential medical information about the care they received, including details about allergies,. If the patient was admitted or transferred to. A hospital discharge form is a form template designed to document patient discharge information and provide evidence of the patient's release from. Discharge summaries are essential documents that ensure continuity of care from hospital to outpatient settings. Include all pertinent lab values and radiology studies here. A discharge form streamlines the discharge process by providing a structured form template that a healthcare provider can quickly fill out with all necessary information, including. Hospital discharge papers template overview. Discharge summary dictated 2 days after discharge states patient went “home”. When a loved one is discharged from the hospital, receiving a comprehensive discharge summary is essential for a smooth transition home. When a loved one is discharged from the hospital, receiving a comprehensive discharge summary is essential for a smooth transition home. Discharge summary dictated 2 days after discharge states patient went “home”. These templates ensure that healthcare professionals can accurately document all necessary details regarding a patient’s condition, treatment, and future care recommendations upon. Hospital discharge papers template overview. If. It includes all the necessary steps to ensure. Discharge summary dictated 2 days after discharge states patient went “home”. Let’s review how to create effective discharge summaries and. Discharge summary forms are usually completed during a patient’s hospital stay and contain essential medical information about the care they received, including details about allergies,. Discharge summaries are essential documents that ensure. Include all pertinent lab values and radiology studies here. Discharge summary dictated 2 days after discharge states patient went “home”. A summary discharge is a comprehensive clinical report prepared by a healthcare professional, typically a physician, nurse, or social worker, at the conclusion of a patient's. A patient discharge form, sometimes referred to as a patient discharge summary, is a. Hospital discharge papers template overview. A summary discharge is a comprehensive clinical report prepared by a healthcare professional, typically a physician, nurse, or social worker, at the conclusion of a patient's. If the patient was admitted or transferred to. Let’s review how to create effective discharge summaries and. Include all pertinent lab values and radiology studies here. If the patient was admitted or transferred to. A nursing hospital discharge checklist template is an important tool used by nurses when discharging patients from a hospital. When a loved one is discharged from the hospital, receiving a comprehensive discharge summary is essential for a smooth transition home. A hospital discharge papers template typically includes several key components, such as. A hospital discharge papers template typically includes several key components, such as patient demographics, admission and discharge. These templates ensure that healthcare professionals can accurately document all necessary details regarding a patient’s condition, treatment, and future care recommendations upon. Let’s review how to create effective discharge summaries and. Physician note on day of discharge further clarifies that the patient will. A hospital discharge papers template typically includes several key components, such as patient demographics, admission and discharge. Include all pertinent lab values and radiology studies here. A summary discharge is a comprehensive clinical report prepared by a healthcare professional, typically a physician, nurse, or social worker, at the conclusion of a patient's. Physician note on day of discharge further clarifies. Hospital discharge papers template overview. If the patient was admitted or transferred to. Include all pertinent lab values and radiology studies here. Discharge summary forms are usually completed during a patient’s hospital stay and contain essential medical information about the care they received, including details about allergies,. Discharge summaries are essential documents that ensure continuity of care from hospital to. A summary discharge is a comprehensive clinical report prepared by a healthcare professional, typically a physician, nurse, or social worker, at the conclusion of a patient's. A nursing hospital discharge checklist template is an important tool used by nurses when discharging patients from a hospital. These templates ensure that healthcare professionals can accurately document all necessary details regarding a patient’s. If the patient was admitted or transferred to. Discharge summary dictated 2 days after discharge states patient went “home”. A nursing hospital discharge checklist template is an important tool used by nurses when discharging patients from a hospital. When a loved one is discharged from the hospital, receiving a comprehensive discharge summary is essential for a smooth transition home. These. Discharge summary dictated 2 days after discharge states patient went “home”. A patient discharge form, sometimes referred to as a patient discharge summary, is a document issued by a hospital to an admitted patient upon discharge. A hospital discharge papers template typically includes several key components, such as patient demographics, admission and discharge. Physician note on day of discharge further clarifies that the patient will be going home with. If the patient was admitted or transferred to. A discharge form streamlines the discharge process by providing a structured form template that a healthcare provider can quickly fill out with all necessary information, including. A hospital discharge form is a form template designed to document patient discharge information and provide evidence of the patient's release from. Let’s review how to create effective discharge summaries and. This document not only outlines. Discharge summary forms are usually completed during a patient’s hospital stay and contain essential medical information about the care they received, including details about allergies,. A summary discharge is a comprehensive clinical report prepared by a healthcare professional, typically a physician, nurse, or social worker, at the conclusion of a patient's. Hospital discharge papers template overview. A nursing hospital discharge checklist template is an important tool used by nurses when discharging patients from a hospital. These templates ensure that healthcare professionals can accurately document all necessary details regarding a patient’s condition, treatment, and future care recommendations upon.FREE 18+ Sample Discharge Summary Templates in Word, PDF
Hospital discharge form template Fill out & sign online DocHub
30 Hospital Discharge Summary Templates (& Examples)
Hospital Discharge Forms 10 Free PDF Printables Printablee
Hospital Discharge Template Sign Templates Jotform
Printable Fillable Real Hospital Discharge Papers
Hospital Discharge Form Flow for Clovis airSlate
30 Hospital Discharge Summary Templates (& Examples)
Hospital Discharge Summary Template Visme
FREE 11+ Sample Discharge Summary Templates in PDF MS Word
Include All Pertinent Lab Values And Radiology Studies Here.
When A Loved One Is Discharged From The Hospital, Receiving A Comprehensive Discharge Summary Is Essential For A Smooth Transition Home.
It Includes All The Necessary Steps To Ensure.
Discharge Summaries Are Essential Documents That Ensure Continuity Of Care From Hospital To Outpatient Settings.
Related Post: